Summary
WICKED (Wolverhampton Interface Care, Knowledge Empowered Diabetes) uses personalised diabetes information to improve self-care. The initiative began by recruiting all local people with diabetes and randomising them into two groups: the active group was mailed a structured personalised report containing information on all 9 of their diabetes care processes while the control group received standard care. Differences in their Failed Process Score (FPS) were compared at three months, where the change was significantly better in those mailed. Patients found this report useful (89%), a source of knowledge (78%) and confidence (74%) and it helped them in understanding their diabetes (78%). Non-responders were at significantly higher risk of developing micro and macro vascular complications.
Results
At 3 months, the FPS score, the change in FPS score, and an improvement in FPS ≥1 were all significantly better in those mailed versus controls. At 3 months the association with Good Attainment (GA, FPS≤1) categorisation was 74% in the mailed group versus 71% in controls. The change in FPS at 3 months was recoded into deterioration, no change or improvement (2924 (20%), 5356 (37%) and 6279 (43%), and, equating this to GA or PA categorisation attainment at 3 months showed significant differences. Patients found this booklet useful (89%), a source of knowledge (78%) and confidence (74%) and it helped them in understanding their diabetes (78%). In non-responders, the FPS was significantly worse as was attainment in every single one of the 9 subsidiary processes. They had a higher HbA1c, BMI, serum cholesterol, Primary CHD risk and were more likely to be smokers.
Challenge
Diabetes care providers target patient activation through the provision of education programmes but these have a very poor uptake: despite NICE guidance only 3% of people with diabetes in the UK have had a structured education programme - and even the best-developed programmes have variable and often disappointing outcomes.
Objectives
To use structured and personalised diabetes information as a tool to activate patients to self-care. To prove that a centrally integrated and validated electronic database to generate person-specific reports was possible in fragmented NHS systems.
Solution
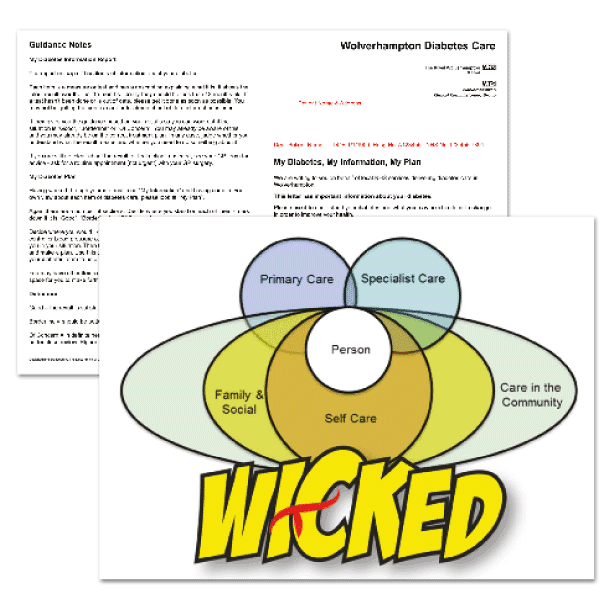
All people over the age of 18 within the local health economy were included in the project, with data captured within the local integrated diabetes information system. The baseline dataset was used to populate a document in an A4 booklet format: ‘My Diabetes, My Information, My Plan’. This was developed by an expert group comprising health professionals, people with diabetes and diabetes educators. It was structured around the key diabetes care processes (and their intended outcomes) containing contemporaneous (within 15 months) individual patient-specific information, with a descriptor for each domain, an assessment of its status (good, borderline, of concern) and brief guidance on potential actions. This fed into a self-assessment (based on ‘Where am I, where do I want to be and how do I get there?’) driven through a reflective adult learning model. People with diabetes were randomised into two groups to either receive the document, which was an active intervention, or not.
Learnings
Rolling out this service development under a robust research framework and applying a research methodology of a randomised controlled trial to obtain objective evidence related to this intervention is an important step. Scarcity of evidence in this arena can make it difficult to learn what benefits patients, but this initiative has provided high quality evidence to support this modern model of diabetes care delivery. Although difficult, it is possible to maintain a centralised electronic diabetes register at a high level of accuracy, and information captured in this register can be used to drive patient care. People with diabetes can understand and utilise their information to construct a meaningful partnership with their healthcare professionals. Once activated to self-care, people can be supported according to their needs and may require much less resources when compared against a standardised service delivery to the whole population. Patient activation requires a behaviour change from healthcare professionals but this is perhaps is the only way forward to maintain a high quality service to people with diabetes, given the increasing prevalence of the disease and limited resources of NHS.
Evaluation
Binary logistic regression analysis was used to compare the relative effect of mailing compared to non-mailing whilst taking into account all demographic factors and the baseline FPS.