Summary
A local psychodermatology clinic has been piloted at St George’s Hospital in South London since March 2022, to support the local community’s skin and mental health needs. A consultant dermatologist and a speciality psychiatry trainee deliver the clinic biweekly, demonstrating consistent patient satisfaction and addressing patients’ needs. The clinic’s success was demonstrable in year one and at reaudit in year two of the service. It is hoped that commissioners will consider formally funding the expansion of this local Skin and Mind service regionally.
Method
The initiative addresses dermatological and mental health needs in one dedicated, physical space. The organisation achieves this by providing the dermatology space and administration to assess and support the referred patients. Delivered by a clinical team of two, over 80 complex patients have been assessed and managed over the past 20 months. Qualitative and quantitative audits of patient outcomes and patient experience have demonstrated consistency in the service delivered and have highlighted the need for a dedicated psychologist to help support this service locally. The Skin and Mind service also encourages trainees from diverse intersectionalities to engage with dermatology-related projects, research and presentations. The service has also helped psychiatric trainees explore this subspeciality formally as part of their psychiatry training. It is hoped that formal funding for the clinic will be obtained by 2024-2025. The clinic lead is in talks with local commissioners regarding this to fund dedicated psychological support formally and to expand the local service regionally for the whole of Southwest London.
Results
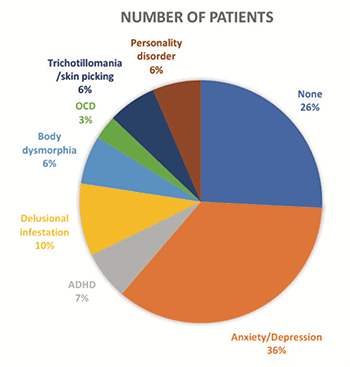
Audits demonstrated that 93% of service users felt they had been listened to and 83% felt understood. Around half of patients said their quality of life had improved and around half felt that they could make the changes suggested. However, a dedicated psychologist (business case pending) could improve this parameter. As a local multidisciplinary team service, significant changes have been made locally while keeping costs at a minimum through effective engagement and signposting to local services. Formal links have been established with the national body dysmorphic disorder and eating disorder clinics to build future collaborations between physical, dermatological health and mental health.
Sustainability and Spread
Service users feel their care is personalised appropriately, with suitable signposting to local services. Themes and risks are often discussed with other clinicians in the department and organisation to feed back on appropriate resources that may be helpful in their daily practice (such as changes in Improving Access to Psychological Therapies services, criteria for referrals to other services, or new social enterprises that are accepting self-referrals). This service promotes and supports opportunities for research to help develop further interest in both dermatology and psychodermatology, while actively supporting opportunities for a diverse group of trainees, addressing tangible health inequalities. The research and lessons learned have been presented at national and international psychodermatology and dermatology conferences.
Psychological Impact of Skin Disease Conditions
Pilot Psychodermatology Clinic in South London
by St George’s Hospitals NHS Foundation Trust