Summary
The ‘Looped In’ initiative pioneered a systematic approach to integrating hybrid closed-loop (HCL) systems into routine NHS care for people with type 1 diabetes. Recognising the challenges of achieving optimal glycaemic control, the team acted swiftly to accelerate access following NICE TA943 guidance. Serving a diverse, socioeconomically deprived population, the programme embedded equity by tailoring education and reducing digital exclusion to ensure representation across the population. Strategic innovations included multidisciplinary team (MDT) meetings and group onboarding which enabled scalable, patient-centred delivery. Published real-world data show improved glycaemic outcomes and patient experience, establishing the service as a model for equitable diabetes technology adoption nationally.Innovation/Novel approach to an existing problem
The ‘Looped In’ initiative adopts a proactive and pioneering approach to integrating HCL systems into routine clinical practice. HCL systems automate basal insulin delivery based on real-time glucose levels, reducing the burden of daily decision-making while improving clinical outcomes. Manchester Royal Infirmery was the first adult diabetes centre in Europe to introduce the first commercially available HCL system in standard NHS care. Therefore, when NICE Technology Appraisal 943 (TA943) promoted widespread adoption of HCL systems the team was well placed to initiate rapid rollout of the ‘Looped In’ initiative. Weekly MDT meetings were held on diabetes technology, identifying eligible individuals and planning HCL initiation. Cross-institutional collaboration with a neighbouring hospital trust upskilled their team. Patient-centred onboarding strategies included group education sessions and structured follow-up. Better integration of administrative and clinical staff streamlined workflows, improving scheduling, ordering of devices and consumables, and resource management. These innovations reflect not just a change in technology, but a fundamental rethinking of how diabetes care can be delivered, to ensure it is scalable, equitable, and centred on lived experience.
Equality, Diversity and Variation
The service covers a socioeconomically diverse and often underserved urban population, with high levels of health inequality. Pathways were designed to reduce variation in access, need, and outcomes. To combat digital exclusion, health literacy, and mistrust of technology the following were delivered: both virtual and in-person onboarding; patients supported by the diverse team in different languages and with use of interpreters; tailored education with one-to-one dietitian and DSN support to overcome health literacy; mobile phones obtained from industry partners. Audits showed that: people from the most deprived quintile were equally represented in the cohort; glycaemic outcomes (TIR, HbA1c) improved regardless of IMD or ethnic group; and patients felt supported and empowered regardless of prior technology exposure or education level.Impact to Patient Care
The Looped In initiative demonstrated significant positive impact, both in clinical outcomes and patient experience. At the time of writing, 1,164 individuals are established on HCL systems. The diabetes centre is located in an inner-city area of Manchester and serves a population that includes some of the most socioeconomically deprived communities in the country. Therefore equity was central to the development and delivery of HCL services. Education, onboarding, and follow-up support were designed to meet the diverse needs of all patients. Improvements in glycaemic control, such as increased time in range and reduced HbA1c, were observed consistently across the cohort, with no association between improvement in glycaemic outcomes and levels of deprivation. Strong emphasis was placed on enhancing patient experience, with group onboarding and continuous patient feedback loops being both efficient and responsive to patient needs and preferences. The one-day group onboarding event highlighted the value of shared learning, peer support, and streamlined training in fostering confidence and engagement with the technology. Feedback from participants showed high levels of satisfaction in both the content and delivery. The approach has been recognised as a leading example of how real-world implementation of diabetes technology can be both evidence-based and equity-focused. The team is committed to scaling the model further and supporting other services in adopting similar approaches.
Results
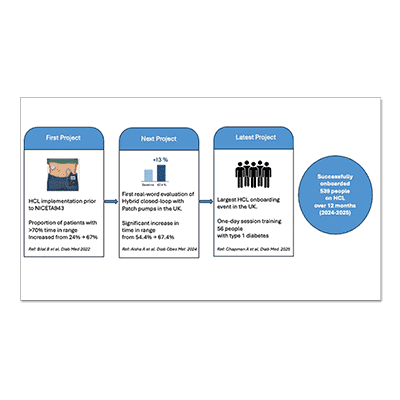
The first project evaluated how the diabetes centre performed with HCL implementation prior to NICE TA943 and was the UK’s first real-world report examining multisystem HCL use within an NHS setting. It included individuals funded by the NHS for insulin pump therapy and real-time continuous glucose monitoring (RT-CGM), transitioning to HCL as part of routine clinical care. After nine months of follow-up, the proportion of individuals achieving the internationally recommended >70% time in range (TIR) increasedfrom 24% to 67%. This improvement was accompanied by a reduction in HbA1c of 4 mmol/mol (p<0.001) after a median of six months using HCL. Next, in 2024, the team published the UK’s first evaluation of the world’s first tubingless/patch HCL system (Omnipod 5) in usual clinical practice. It showed a significant increase in TIR from 54.4 ± 17.4% to 67.4 ± 14.3% (paired difference +13%, p < .001). Time spent above 10 mmol/L dropped from 43.0 ± 18.2% to 31.1 ± 15.0% (−11.9%, p = .005), and time spent <3.9 mmol/L reduced from 2.0% (1.0, 3.0) to 1.0% (0.0, 2.0), p = .004. Importantly, there was no correlation between improvement in TIR and the deprivation index (r = 0.05, p = .7), indicating benefits were consistent across socioeconomic backgrounds. The most recent project demonstrated that large-group HCL training and onboarding can be delivered in an NHS setting with careful planning and support. The aim was to develop scalable solutions to meet increased demand. The team delivered the UK’s largest single-day HCL onboarding event in collaboration with clinical, administrative, and industry partners. It trained 56 people with type 1 diabetes, supported by diabetes specialist nurses. Feedback questionnaires showed that 96% felt the event met their expectations, 94% felt adequately trained, and 98% would recommend the event to others. In 12 months (2024-2025), 539 people were onboarded onto HCL. This initiative provides a replicable framework.User Feedback
Anonymised questionnaires and direct interactions with clinical educators provided overwhelmingly positive responses. Feedback highlighted the effectiveness, clarity, and accessibility of the large group onboarding format. A significant outcome has been a substantial reduction in waiting times for initiating HCL therapy from up to 12 months to within one month for most systems.