Summary
In 2018 Cardiff and Vale (CAV) UHB introduced a ‘walk-in clinic’ (WIC) for patients with diabetes and a foot emergency. This service, while successful, needed to adapt to meet the demands of the health service. A pilot ‘phone first’ diabetic foot emergency early triage (DFEET) service was trialled, where patients living with diabetes with a foot emergency could contact the department, speak to a triaging podiatrist and be offered advice and an appropriate appointment. The service is a ‘one-stop shop’, with access to interventions such as X-rays, microbiological sampling, independent prescribing and MDT access.
Innovation
The 2018 WIC ran twice weekly but, despite increasing to three times a week, its format did not meet current demand and was unsustainable. The aim was to enhance and expand the offering of urgent care by changing to a community-based, ‘phone first’ DFEET system offering virtual consultations with a triaging podiatrist and appropriate appointments. The service also provided a ‘one-stop shop’ with access to investigations such as X-rays, microbiological sampling and phlebotomy, plus timely access to antibiotics using patient group directives and independent prescribing. The plan was to reduce the numbers of patients waiting longer than three days for their first expert assessment by 20% within the project cycle, to prevent inappropriate A&E attendance and GP contact for diabetic foot-related emergencies and, longer term, to offer phone-first contact to all patients with foot wounds. Using a PDSA approach, a pilot service commenced one day a week, running alongside WIC for six months prior to moving to DFEET four days a week. Co-design with stakeholders was central and a focus group was held with patients to capture views on the changeover.
Equality, Diversity and Variation
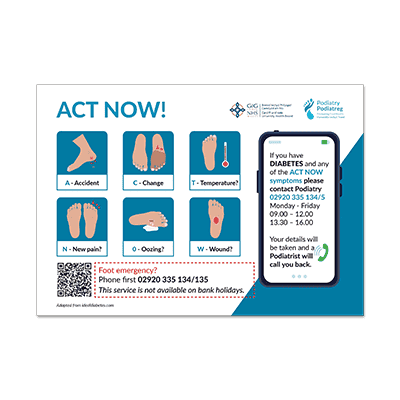
DFEET supported the Equality and Diversity Act (2010) and the NHS equality, diversity and inclusion improvement plan. DFEET also aligned with the Podiatry Strategy 2022-2024 with the incentive to promote equality in health and well-being for all by targeting health inequalities. It also supported the Well-being of Future Generations (Wales) Act, contributing to the cultural well-being goal by increasing the number of Welsh speakers to allow patients to interact in their chosen language. It utilised the Wales Interpretation and Translation Service to provide linguistic services to provide improved quality and safety in interpretation and translation for all cultures in face-to-face appointments. ACT Now leaflets designed by the podiatry service were developed with equality and diversity in mind, with cultural appropriation in the images. Embracing technology and digital communications for triage freed clinical locations and appointments in face-to-face clinics closer to home. Future ambitions include expanding the phone first service to a five-day working week for all pathologies, not just the diabetic foot. A business case will be submitted to ensure funding and clinical capacity to initiate this expansion. DFEET was provided to all, regardless of age, gender reassignment, disability, race, religion, sex and sexual orientation.
Results
In total, 320 patients were reviewed by the DFEET service in a seven-month period between July 2023 and January 2024. A total of 93.4% (n=299) patients were seen within three days of referral, with 6.6% (n=21) waiting longer than three days. This was a 30.4% reduction in the number of patients waiting longer than three days, compared with NDFA data from 2021-2022. In terms of clinical outcomes, 115 patients had a new active foot ulcer, 47.7% (n=52) of whom were alive and ulcer-free at 12 weeks. A total of 24.8% (n=27) had an unhealed ulcer, 0.9% deceased (n=1), 26.6% (n=29) were lost to follow up or no outcome was recorded. The average healing rates of all ulcerations nationally is 26% and DFEET recorded a 50% healing rate. In terms of reducing A&E and primary care appointments, 59% (n=240) of patients who attended a DFEET clinic stated they would have attended a GP appointment if DFEET did not exist and 5% (n=21) stated they would have attended A&E. Of 324 patients attending the DFEET service, 115 attended a GP appointment first and were then referred to DFEET. This cost the NHS two separate appointments for the same pathology. DFEET wants to eliminate duplicate appointments and offer a one-stop shop. Of the 324 patients, 74 were seen by the practice nurse before referral to DFEET. Only six patients attended A&E before being referred to DFEET. Considering the costs of patients attending primary care services prior to, or instead of, the DFEET service, DFEET saved £14,177 a year.
User Feedback
Out of all responses from GP surgeries, 55% reported that they had used the new DFEET system and were positive about the initiative. However, only 36% of ACT Now DFEET posters were advertised in waiting rooms. Rating the service from 1-5, the average mean rating was 4. Feedback from primary care services acted as a motivational tool for all DFEET staff to believe in and support the project. This feedback was delivered to healthcare staff to applaud their clinical performance over the seven months. A patient experience questionnaire was used in person to allow patients to consent, understand and digitally complete the survey. Paper copies were provided for those who were not literate in digital technology. The form was devised to collect data throughout the DFEET journey.
Dissemination and Sustainability
One of the aspirations of the project was to promote sustainability with digital technologies to support appropriate use of high-risk clinics. This redirection and reduction of interventions with the highest skilled members of the podiatry team and duplication within the podiatry service helped to reduce delays in appropriate care, variation and waste. Despite data signalling a reduction in GP and A&E visits, further work is needed in primary care to ensure that patients present at the earliest convenience. Cost-benefit analysis showed DFEET will decrease money spent on diabetic foot ulcers in primary care. Incorporating virtual technology was an integral asset in the DFEET clinic. Use of virtual consultations for effective triage reduced the need for expert assessment in DFEET by 31%.