Summary
Traditional models of routine follow-up out-patient care are widely recognised to be inefficient and often ineffective as they fail to reliably provide responsive care when patients need intervention. This project aimed to provide more accessible and cost-effective diabetes care by replacing routine follow-up out-patient appointments for patients who don’t require physical examination with web-based consultations. It used everyday technology available in people’s homes and included patients of all ages from ethnically diverse communities conducted in an urban inner-city environment. From January 2011 to the time of entry, 234 online appointments had been conducted. Trends support the qualitative data showing patients who have had several webcam appointments have a reduction in HbA1c levels with fewer A&E attends. A two-year study is now ongoing exploring the role of web-based consultations in improving self-management.
Results
Recruitment figures show that there was little variation in acceptance of web-based consultations for those under the age of 50 – the overall acceptance across age and ethnicity was 62% (an initial trial with Adobe Connect was rejected in favour of Skype software).
Patient feedback was obtained from19 in-depth telephone interviews, a focus group and 28 on-line questionnaires. Findings indicated web-based appointments are convenient and often preferable to patients who report they ‘feel more in control’ with no difference in their quality of care.
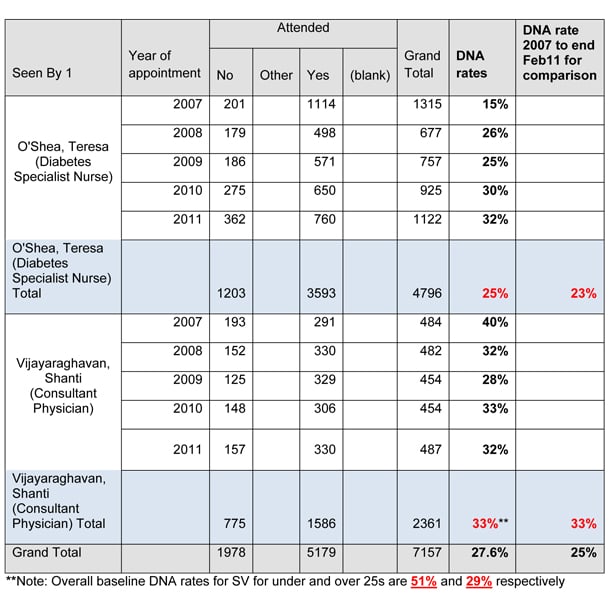
Clinic DNA rates have reduced from 27%, to 16%. Patients using web-consultations had 12 diabetes-related A&E attendances in the year pre-intervention and none subsequently, but longer-term data is required before conclusions can be drawn.
In-patients who received more than two online consultations showed an average HbA1c reduction of 1.65%, suggesting greater medication compliance and better self-management.
Challenge
The prevalence of diabetes in Newham is 6.9%-9.9%, around 5-6 times the national average, and due largely due to the local BME population. Rates are projected to increase to 13.5% by 2030.
There are currently 14,000 patients on the local diabetes database (DIAMOND) and the prevalence of Type 2 diabetes in young people is about 4-5 times the national average. The antenatal clinic managed 420 diabetes related pregnancies in 2009/10.
The Borough has high levels of socioeconomic deprivation and this, coupled with cultural factors, leads to poor self management with high non-attendance rates and poor health outcomes.
The Department of Health You’re Welcome (2009) initiative highlighted inflexible services as the leading cause of missed appointments, especially for people in education or employment, or those with carer responsibilities or language problems. Local broadband usage is 70% (63 % national), probably reflecting the needs of this multi-ethnic population. Following a small technology audit with NHS Choices, questionnaire-based surveys were conducted to determine general broadband use and the acceptability of remote consultations. Funding was then obtained to explore web-based consultations in routine diabetes care.
Objectives
It was anticipated that web-based consultations would improve the efficiency of the outpatient process, enhance patient self-management skills and be cost effective. This would be achieved by: Lowering the cost per outpatient contact; reducing the number of missed appointments (DNAs) and demonstrating improved health outcomes because of a more proactive approach to self-management with a concomitant reduction in attendance at emergency services or use of out-of-hours facilities. It would also reduce costs for patients having to travel or take time away from work or other commitments, reduce the amount of time they needed to allocate for consultations and offer greater convenience.
Solution
Suitable patients attending routine follow-up diabetes appointments were offered web-based consultations, where physical examination was not required, using readily available video-conferencing software. Outcome data including DNA rates, clinical measures, financial impact and staff and user satisfaction were recorded.
Since January 2011, 234 online appointments have been conducted (62% uptake across all ages and ethnic groups) with a DNA rate of around 27%, which is decreasing with time as patients adapt to a new system. Patients report web consultations are more convenient, cheaper and more likely to be kept. Staff and patients report that the quality of online care remains at least as good as that provided face-to-face.
A core working group, involving outpatient administration staff, ICT managers and clinicians was set up and met regularly during the project, allowing operational problems to be addressed immediately.
A strategic project Board, involving internal and external stakeholders, met quarterly ensuring support from key partners, and embedding of the project.
Evaluation
More time is needed to verify quantitative findings but early indications are that patients who have had several webcam appointments have reduced HbA1c levels, fewer A&E attendances and there are modest efficiency savings. There have been documented savings for patients (where the service impacts on earnings) and wider societal benefits.
Patients of varying age and ethnicity preferred webcam appointments and say they were more likely to attend. The choice of software provider is important for ease of use and reliability.
The initiative is already showing more focused consultations, a reduction in patient transport and staff travel, and findings suggest DNA and A&E attends will reduce with time, with associated cost benefits. More significant savings will result from reduced out-patient infrastructure costs with increased online follow-up.
Impact
It is evident that people in employment or education, younger patients, those homebound or with carer responsibilities have benefited most. Our patients now use laptops, phones and iPods for online follow-up.
The staff benefits from improved efficiency, reduced travel time and greater user satisfaction. The project has attracted widespread media attention, interest from other NHS organisations and a recent visit from NHS
England.
Increased use of online follow up within the diabetes service is planned for in-patient and community nursing teams and a pre-pregnancy service. A clinical group has been established to explore wider use within the merged Barts Health NHS Trust and the system is already being used by surgical specialist nurses.